The PIP implant scandal has been rumbling on, with no resolution, for a protracted period now.
It’s exactly two years since France’s health regulator, AFSSAPS, ordered the withdrawal of silicone breast implants made by PIP.
But the issue only reared its head in the UK at the back end of 2011 – 21 months after AFSSAPS and indeed, its UK equivalent the Medicines and Healthcare Products Regulatory Authority (MHRA) knew they were substandard.
Last week, the Commons health select committee stated that the UK government response has been “inadequate”. As if to compound this, MHRA head, Sir Kent Woods (speaking in front of the committee), admitted he could not give an assurance that no PIPs were implanted after the 2010 withdrawal. “One sincerely hopes that it did not happen,” he said sheepishly.
Latest figures suggest that the total number of women affected in the UK is 47,000; 95% of women had the operation privately, 5% on the NHS.
There is a whole maelstrom of issues tied up with PIPs. Who is responsible for removing them? Indeed, should they be removed?
At its heart is data; numbers, costs, medical research, timelines. All of which seem impossibly hazy – particularly when it comes to analysing the long-term health consequences of having industrial-grade silicone inside your body.
But in addition to the statistical emphasis, this story has deep emotional resonance. Irrespective of your thoughts on breast augmentation, you can’t dispute the immorality of a) sanctioning the use of PIPs in the first place and b) allowing their use to continue in full knowledge of the possible dangers.
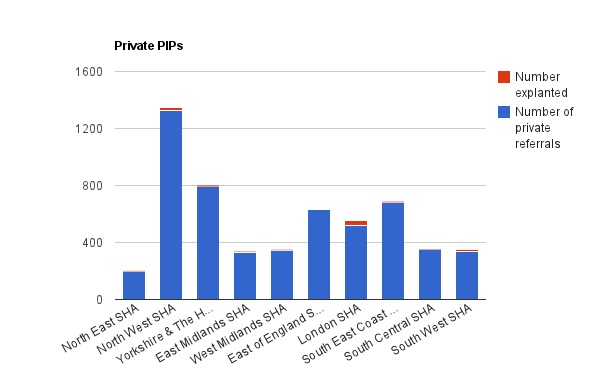
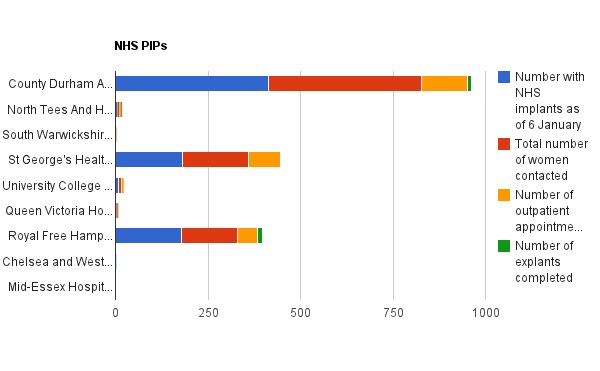
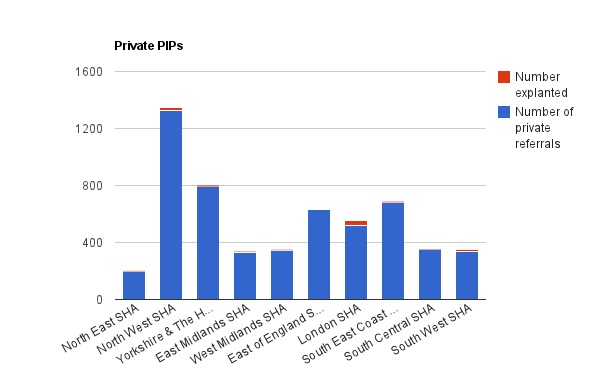
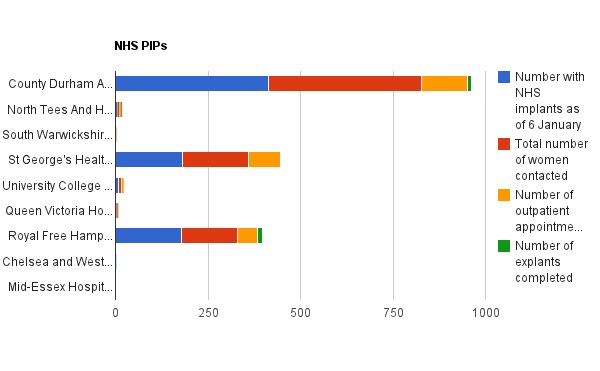
Since January the Department of Health has been releasing bi-weekly data collections monitoring the “NHS Offer” in England; one set monitors the number of private PIP patients who have presented to the NHS, the other tracks women who have PIP implants implanted by the NHS.
The stats are interesting in light of the ruckus last week – that women face two operations instead of one due to NHS small print.
Over 5000 women have been referred to the NHS from private companies including Transform and Harley – but under 100 thus far, have had their implants removed.
And as for the NHS treated patients, a tad under 800 women are reported to have PIPs as of 6 January (the first release date for the stats).
The data is interesting also because of what’s not here. What of the other 40,000 women with PIPs who haven’t presented for a referral? A proportion, I guess won’t be in England. Some of will be treated privately. Some will chosen not to have their implants looked at.
And why, is the NHS data drawn from a very limited number of trusts (a meagre nine)? Did only nine use PIPs? If so, why?
So many questions – a few posts-worth – are remaining, about the ethical issues, as well as the data.